If you’ve had a look through our website, or know about our Demand Diversity campaign, you’ll be familiar with our mission to improve diversity within clinical trials. While this remains a complex issue that requires a range of approaches to achieve real, long-term change, there is so much you can be doing already. It’s time to take a step back and consider one of the roots of this issue: bias.
What exactly can bias mean here?
- Implicit bias describes associations or attitudes that influences someone’s perceptions and actions, though the person themselves remains unaware.
- On the other hand, conscious bias stems from discriminatory beliefs and values that a person holds.
In clinical research, conscious bias is extremely dangerous. The Tuskegee Study is just one example of how conscious bias, which manifested in the form of racism, allowed unethical experiments to take place. When not addressed, implicit bias can also have equally detrimental consequences, including miscommunication, mistrust, decreased satisfaction and disempowerment1. Sadly, research suggests that implicit bias still silently seeps through healthcare today2.
How does implicit bias affect us?
As most societies become more diverse, healthcare professionals are increasingly faced with the need to interact effectively with and provide care for patients whose cultural background may differ from their own. A healthcare professional’s implicit bias about particular characteristics, along with inadequate cross-cultural communication skills, may contribute to less effective medical care and health disparities between different patient populations2. Healthcare professionals themselves may not be racially prejudiced, but healthcare services and institutions may operate in a way that discriminates against certain groups due to embedded norms, values and practices.
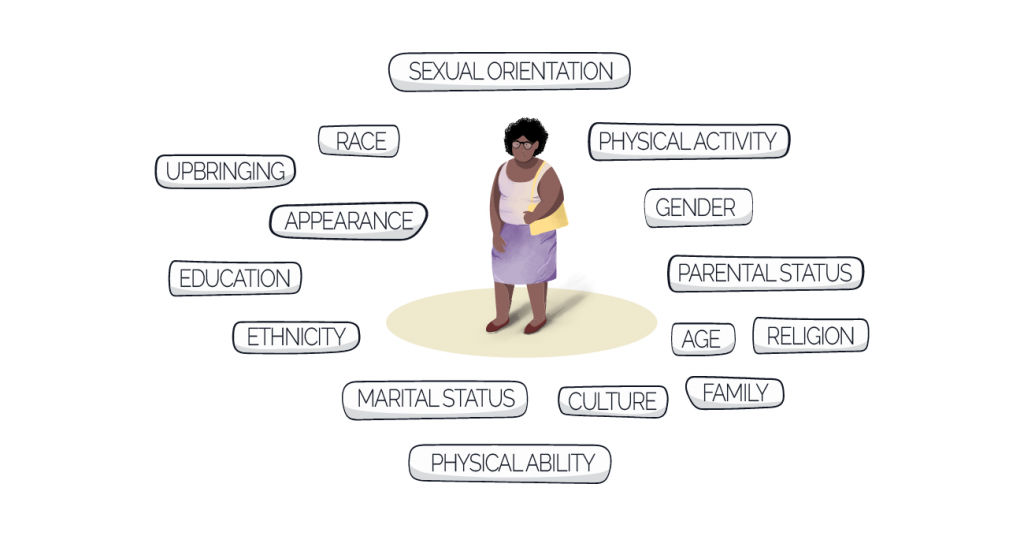
It’s important to emphasise that healthcare professionals may think they are behaving and communicating in a culturally safe manner, when in fact they are not. They may also just lack the necessary training in cultural safety (more on that below!). For example, one study found over 80% of healthcare workers often or sometimes found it more difficult to engage with or treat patients from cultures different to their own3. Furthermore, many may fail to consider how many elements come under the cultural umbrella.
You can’t just think about ethnicity and think that’s the job done.
Implicit bias in clinical trials
And of course, implicit bias can extend to clinical trials. Everyone in healthcare needs to understand the different parts of someone’s culture that could influence their interactions and experiences with clinical trials.
Could site staff in your study be unknowingly expressing bias and negatively impacting patient recruitment? Maybe your site staff aren’t exhibiting bias, but could benefit from training that would help them bring down the barriers that stop underrepresented groups from taking part. Or maybe, those working on patient materials for your study aren’t considering the impact design and content can have on diversity and inclusion. You need to make sure everyone involved in your study has the tools necessary to succeed.
Although it’s an undeniably negative situation, it can be addressed and rectified. How you ask?
Say hello to cultural safety training.
Cultural safety to the rescue!
You may have heard about this before, or perhaps you’ve heard of cultural competency? Although they are similar, there are differences between the two approaches.
- Cultural competency is the ability to understand, communicate and effectively interact with people across different cultures.
- Cultural safety encompasses all of these points but goes further, and explores healthcare professionals’ individual attitudes, biases, stereotypes and more4.
Training in cultural safety allows people to evaluate and critique these characteristics to become more self-aware, and to ultimately provide the best possible care to everyone. Cultural safety training also encompasses improving cultural awareness and understanding. It’s been found that practitioners’ increased cultural competence has been linked to increased patient satisfaction, treatment adherence and information seeking and sharing1.
Cultural safety for those working in clinical trials can help overcome the lack of diversity within participants, by removing some of the barriers to underrepresented groups taking part. Examples of sessions you might expect to see in a robust cultural safety training programme include:
- The importance of cultural safety in clinical trials
- Understanding the patient perspective
- Health literacy and language barriers
- Education on health system bias
- Using the right terminology
- Tools to develop culturally safe clinical trials
Cultural safety training should never be a quick online meeting. It is a long process that needs a combination of training sessions, practice scenarios and experiences in the real world.
Yes, your clinical trial population might be far from diverse and inclusive at the moment. But by taking a step and tackling one of the root causes with cultural safety as the antidote, you can make a positive change sooner than you think.
Get started now
As an industry, we need to ensure that anyone involved in healthcare communicates effectively and compassionately with patients and caregivers. And that those who decide how health information is provided or communicated are equipped to do so in a culturally safe manner.
Are you ready to ensure everyone working on your clinical trial is empowered to do just that? Get in touch to find out about our cultural safety training here at COUCH Health.
References
- Jongen C, McCalman J, Bainbridge R. Health workforce cultural competency interventions: a systematic scoping review. BMC health services research. 2018;18(1):232-232. doi:10.1186/s12913-018-3001-5
- FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Medical Ethics. 2017/03/01 2017;18(1):19. doi:10.1186/s12910-017-0179-8
- Shepherd SM, Willis-Esqueda C, Newton D, Sivasubramaniam D, Paradies Y. The challenge of cultural competence in the workplace: perspectives of healthcare providers. BMC Health Services Research. 2019/02/26 2019;19(1):135. doi:10.1186/s12913-019-3959-7
- Curtis E, Jones R, Tipene-Leach D, et al. Why cultural safety rather than cultural competency is required to achieve health equity: a literature review and recommended definition. International Journal for Equity in Health. 2019/11/14 2019;18(1):174. doi:10.1186/s12939-019-1082-3